What is digital mammography?
October 8, 2024
The difference between mammography and ultrasound
October 8, 2024Mammography is an essential tool for breast cancer screening and diagnosis. Using low-dose X-rays, doctors can detect abnormal areas or tissue in your breast, which can help detect cancer before symptoms appear.
Of course, abnormal breast tissues are often non-cancerous or benign.
Mammography plays a key role in breast cancer screening. Through it, doctors can detect breast cancer before it causes signs and symptoms. Research has shown that mammograms reduce the risk of dying from breast cancer.
A conventional mammogram creates two-dimensional images of the breast.
Another type of mammography called 3D mammography (breast tomosynthesis) creates 3D images of the breast.
Many medical centers offer 3D mammography in addition to 2D mammography for breast cancer screening.
Different types of digital mammography
In general, there are two main types of mammography:
Digital mammography in two dimensions
Digital mammography in three dimensions (digital breast tomosynthesis).
Digital mammography
In the United States, digital mammography has replaced conventional (film) mammography, also known as analog mammography. Both digital and conventional mammograms use X-rays to produce an image of the breast.
Comparison of analog and digital mammography:
The difference is that the image is stored directly on film in a conventional mammogram, while a digital mammogram provides an electronic image that is stored as a computer file. Digital mammography allows healthcare providers to store the file electronically and easily review and share the images. Digital mammography usually includes at least two images of each breast taken at different angles. It usually provides a two-dimensional view from top to bottom and from one side to the other.
Some imaging centers in Iran still have analog mammography systems or first generation digital mammography systems (CR), in which cassettes are used. Golestan Radiology is proud to use advanced generations of digital mammography (DR), in which flat panels are used and images are interpreted by special mammography workstations.
۳D mammography
۳D mammography, called digital breast tomosynthesis (also known as DBT), is a new type of mammography in which each breast is compressed once. The machine moves in an arc over your breast and takes several low-dose x-rays. A computer then stitches the images together, which allows healthcare providers to see your breast tissues clearly in three dimensions.
Many studies have shown that 3D mammography increases the detection of cancer, including low-grade cancers, and reduces the rate of false-positive mammography. Due to these advantages, 3D mammography is rapidly becoming an alternative to 2D mammography for screening and diagnostic mammography.
Preparation for mammography:

Schedule the test for a time when your breasts are least sensitive. If you have your period, usually during the week after your period is a good time.
Bring your previous mammography images or mammography CD.
Avoid using deodorants, antiperspirants, powders, lotions, creams, or perfumes in the armpits or on the chest before the mammogram. Metal particles in powders and deodorants can be visible in your mammogram and confuse the doctor.
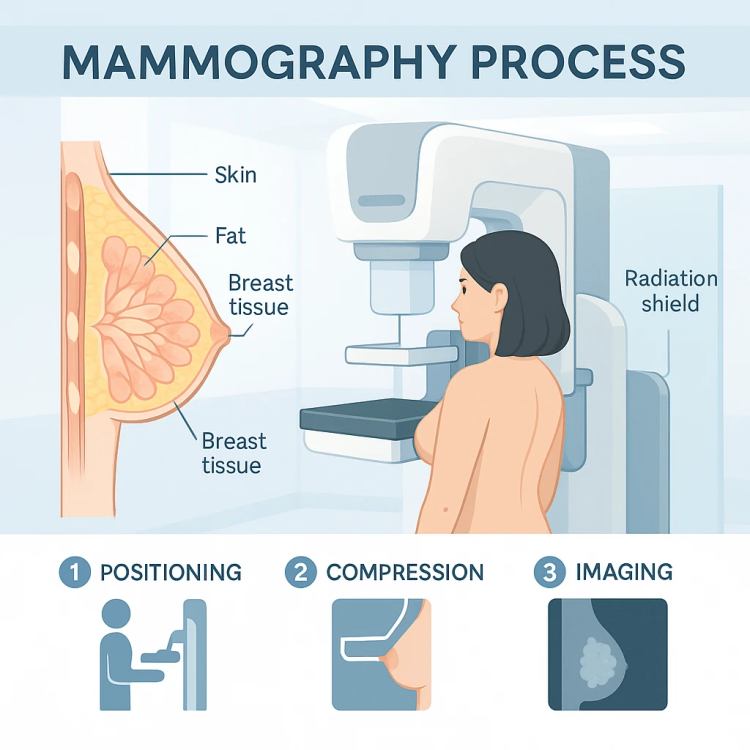
How does mammography work?
A mammogram uses X-rays and is designed only to examine breast tissue. The amount of X-rays produced in this device is much less than the X-rays produced in radiology devices that are used to examine, for example, bones or other areas of the body.
During a mammogram, you place your breast on a support plate attached to an X-ray machine. A technician will then measure your chest with a parallel plate called a paddle press. The X-ray machine produces X-rays, and after passing through the breast tissue, it hits a detector. The detector sends electronic signals to a computer to form a digital image. These images are called mammography.
Pressure on the chest is not harmful, but it can cause some degree of pain. If the pain becomes too much, tell your healthcare team. Your breast should be compressed to even out the thickness and allow the x-rays to penetrate the breast tissue. The pressure also holds your breast still to reduce image blurring from motion and minimizes the required radiation dose. During the short X-ray exposure, you will be asked to stand still and hold your breath.
After images are taken of both breasts, you may be asked to wait while the care team reviews the quality of the images. If the views are insufficient for technical reasons, you may have to repeat part of the test. The whole procedure usually takes less than 30 minutes. After that, you can get dressed and resume your normal activities.
Mammography answer

You will likely receive your mammogram results within a few days, although this may vary. The radiologist will review your mammography and then send the results to you and your doctor.
Breast imaging data analysis and reporting system (BI-RADS)
Radiologists and physicians rely on a standardized system in medical reporting to describe screening and diagnostic mammography findings called the Breast Imaging Data Analysis and Reporting System.BI-RADS) are used. This system divides the results into the following number categories:
imperfect (BI-RADS 0)
This result means that the radiologist may have seen the possible abnormal area, but will need specialized imaging, such as a diagnostic mammogram or ultrasound, to evaluate it. It may also mean that the radiologist will want to compare your most recent mammogram with older mammograms to see if the area has changed over time.
negative (BI-RADS 1)
This result means that the radiologist did not find a significant abnormality to report. Your breasts have no lumps, changes in structure, or suspicious calcifications. A negative in this case means that there are no abnormal areas or findings.
Benign findings (non-cancerous) (BI-RADS 2)
This result means that the radiologist has found a benign (noncancerous) structure in your breast, such as a benign calcification, cyst, lymph node, or fibroadenoma. The radiologist records this finding to help compare it with future mammograms.
Probably benign finding (BI-RADS 3)
This result is given only after diagnostic mammography. Findings in this category have more than 98% chance of being benign (non-cancerous). But since it hasn’t been proven to be benign, the radiologist will want to monitor it to make sure it doesn’t change over time. You will probably need another mammogram in six months.
suspected abnormality (BI-RADS 4)
This result is given only after diagnostic mammography. This means the findings may be cancer, but the radiologist will recommend a breast biopsy for more information. Findings in this category can have a wide range of levels of suspicion and are sometimes divided into other categories, including:
۴A: Low chance of cancer
۴B: Moderate probability of cancer
۴C: High probability of cancer
highly suggestive of malignancy (BI-RADS 5)
This result is given only after diagnostic mammography. The term “malignant” refers to the presence of cancer cells. This result means that the findings are similar to cancer and have at least a 95% chance of cancer. The radiologist strongly recommends a breast biopsy.
Known biopsy-proven malignancy (BI-RADS 6)
Radiologists use this result only for mammogram findings that have already been diagnosed as cancer by biopsy. Doctors use mammography in this way to see how well the cancer is responding to treatment.